Osteopaths understand that everything in the body is connected. This even goes beyond muscles, joints,…

Fibromyalgia
Fibromyalgia is a poorly understood condition. Its name literally means “painful muscles and soft tissues” but there’s more to it than that.
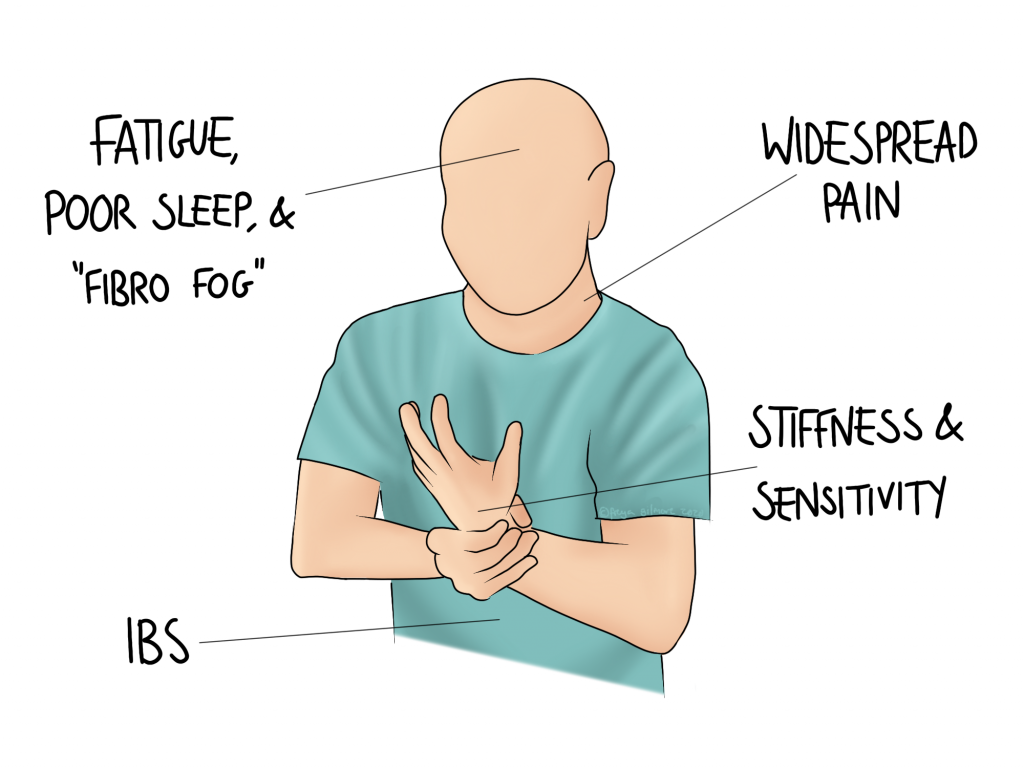
Symptoms of Fibromyalgia
The condition affects women more than men. It is characterised by widespread chronic pain, but also sleep disturbance, fatigue, and cognitive dysfunction. It may develop after a stressful or traumatic period, or there may be no obvious trigger. Symptoms are inconsistent, often with no perceivable pattern. However, the condition is not progressive, and does not cause tissue damage. Patients may find that gentle exercise helps to reduce symptoms, and that stress makes them worse.
Anxiety and depression are common complications of fibromyalgia. Management with antidepressants may improve both the mental health and other symptoms. Talking therapies can also help.
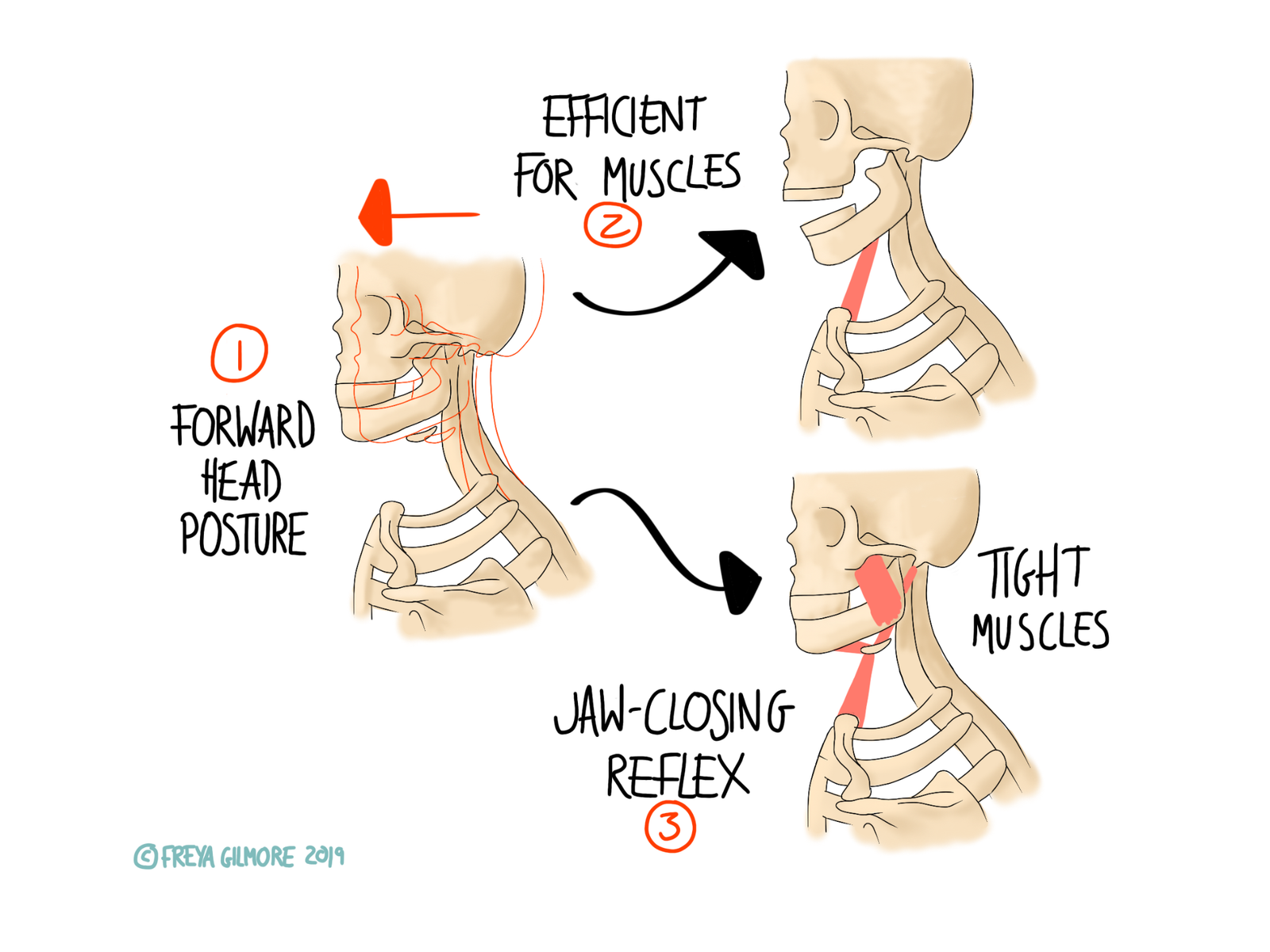
Other musculoskeletal conditions are associated with the condition, such as:
- TMJ (jaw) problems
- Osteoarthritis
- Carpal Tunnel Syndrome
- Hypermobility
- Rheumatoid Arthritis
- Migraine
A Functional Condition
Fibromyalgia is functional. This means that it cannot be diagnosed on MRI or X-Ray, as nothing structural will show up. There is also no inflammation within the painful tissues, nor any damage there. Instead, it is diagnosed by ruling out other potential causes, along with a set of criteria.
In the past, we used a pattern of painful areas to identify the condition. This is now considered outdated in some circles. We still use the old criteria of widespread pain (upper and lower body, and left and right side), that is chronic (over three months duration). A new criteria to address symptoms beyond pain is now recommended on top of this. This system uses a ranking scale to assess the severity of fatigue, unrefreshing sleep, and cognitive difficulty.
IBS is another example of a functional condition: scans, biopsies, and blood tests will show nothing, but that doesn’t mean the symptoms aren’t there. Interestingly, IBS is more common in people with fibromyalgia than the general population.
Pain Science
The cause of fibromyalgia is not yet determined. The type of pain involved is not fully understood either. The general consensus is that there are three types of pain:
- nociceptive: the most simple kind of pain- where you hurt yourself and it causes pain. A twisted ankle would be an example of this. It doesn’t last long and leaves no lingering pain after it heals.
- neuropathic: slightly more complicated but still relatively straight forward. In conditions like sciatica, a nerve is irritated, which can cause strange symptoms. Rather than pain local to the injury, there might be shooting pain along the length of the nerve. There might also be pins and needles, numbness, or weakness.
- central sensitisation: when pain becomes chronic, the nervous system can begin to process it differently. This makes it harder to shift, and comes with new symptoms. You may become hyper sensitive to painful stimuli, and also feel pain from typically non-painful things. An example of the latter could be pain from bedsheets moving over your skin.
However, fibromyalgia doesn’t completely follow any of these patterns. Sensitisation might come close, but still doesn’t explain the symptoms beyond pain.
Osteopathy for Fibromyalgia
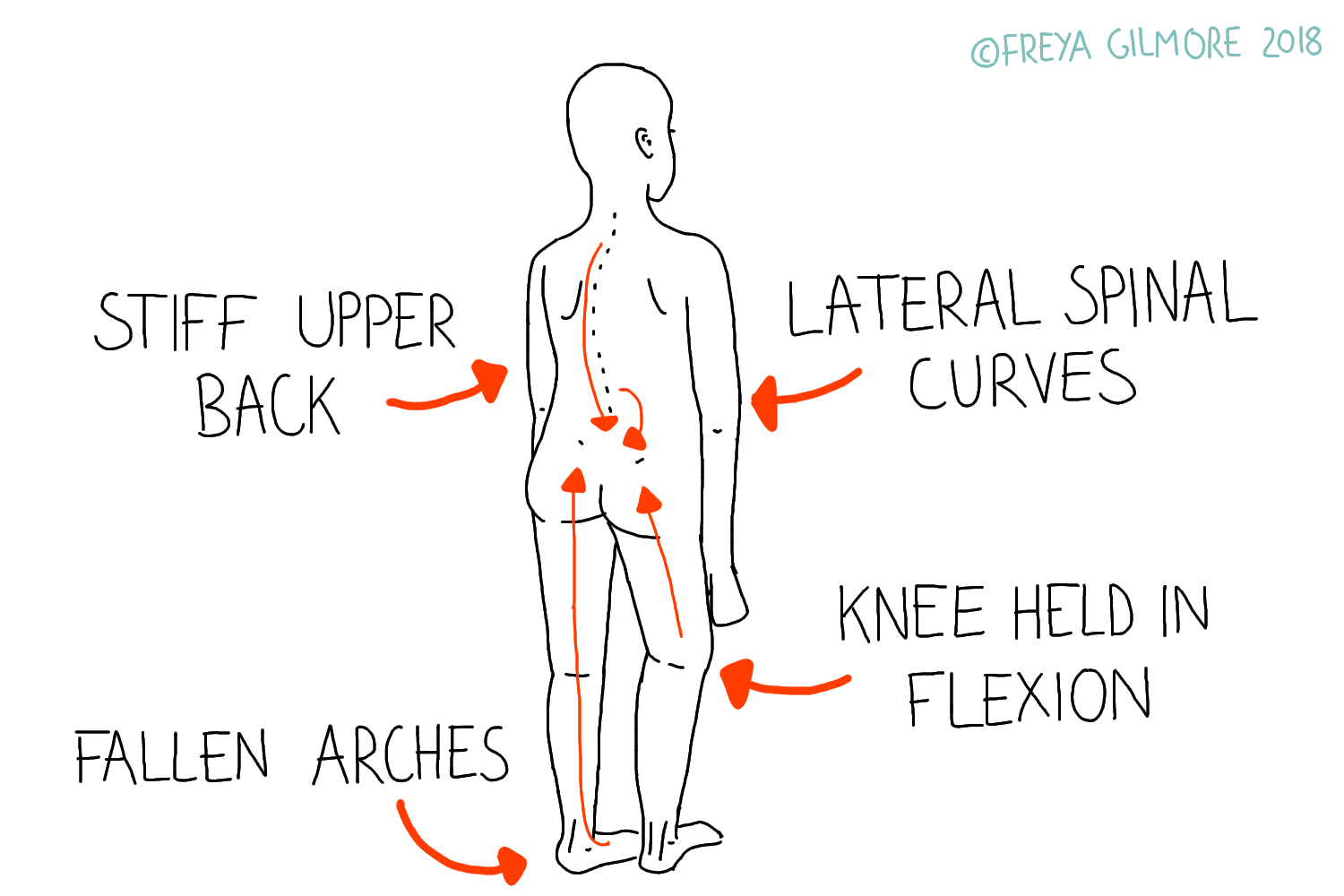
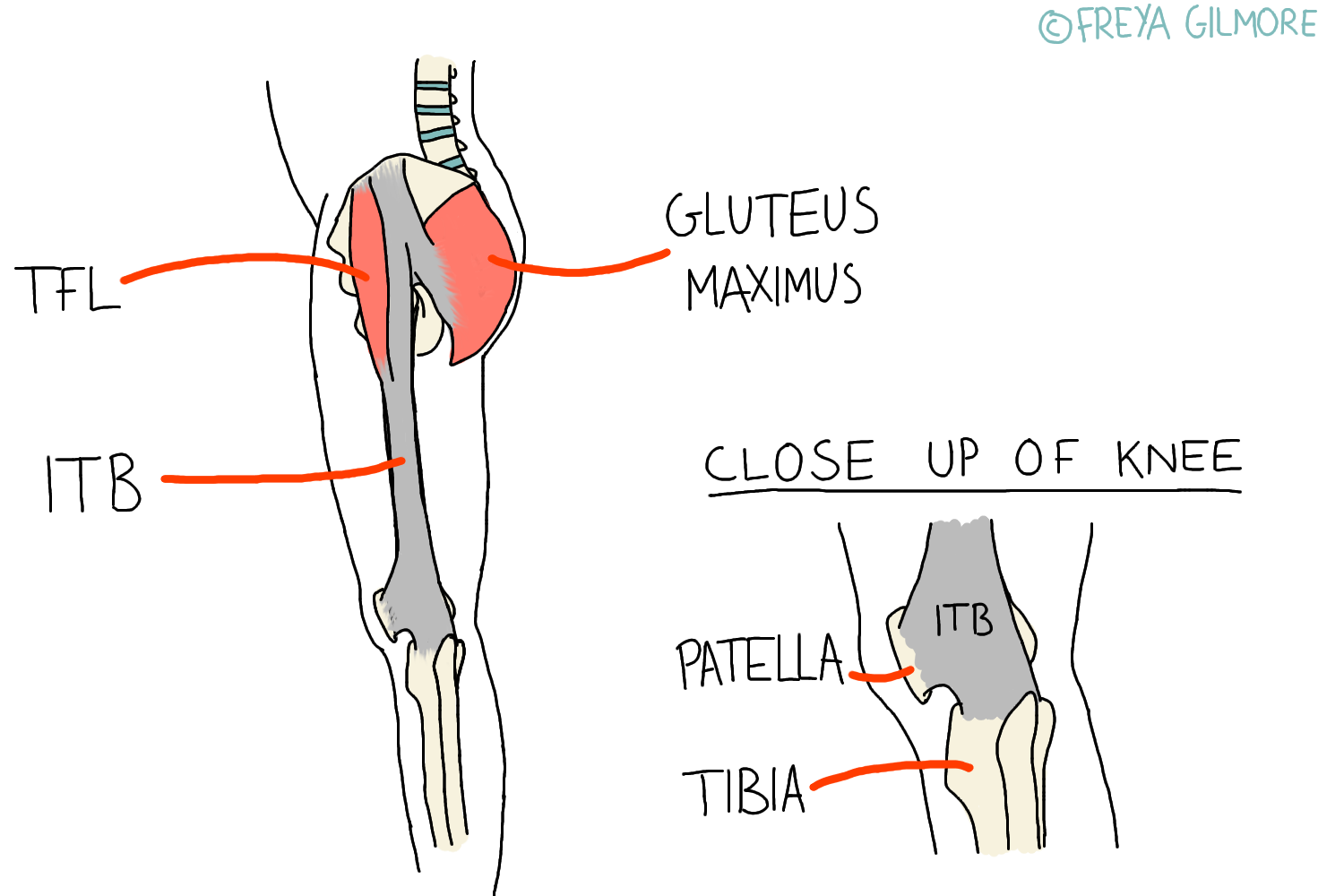
Some patients find that osteopathy helps to improve their quality of life. Gentle treatment to the soft tissues may help relieve some muscular pain, and can sometimes begin to calm down some of the pain response. We may also be able to help manage secondary problems caused by the pain and stiffness. If joints are stiff and sore, you are inclined to move them less, which can reduce the health of the joint in question. We can help with preventative management of arthritis.
If you suffer from the symptoms of fibromyalgia, make an appointment here and see how we can help.