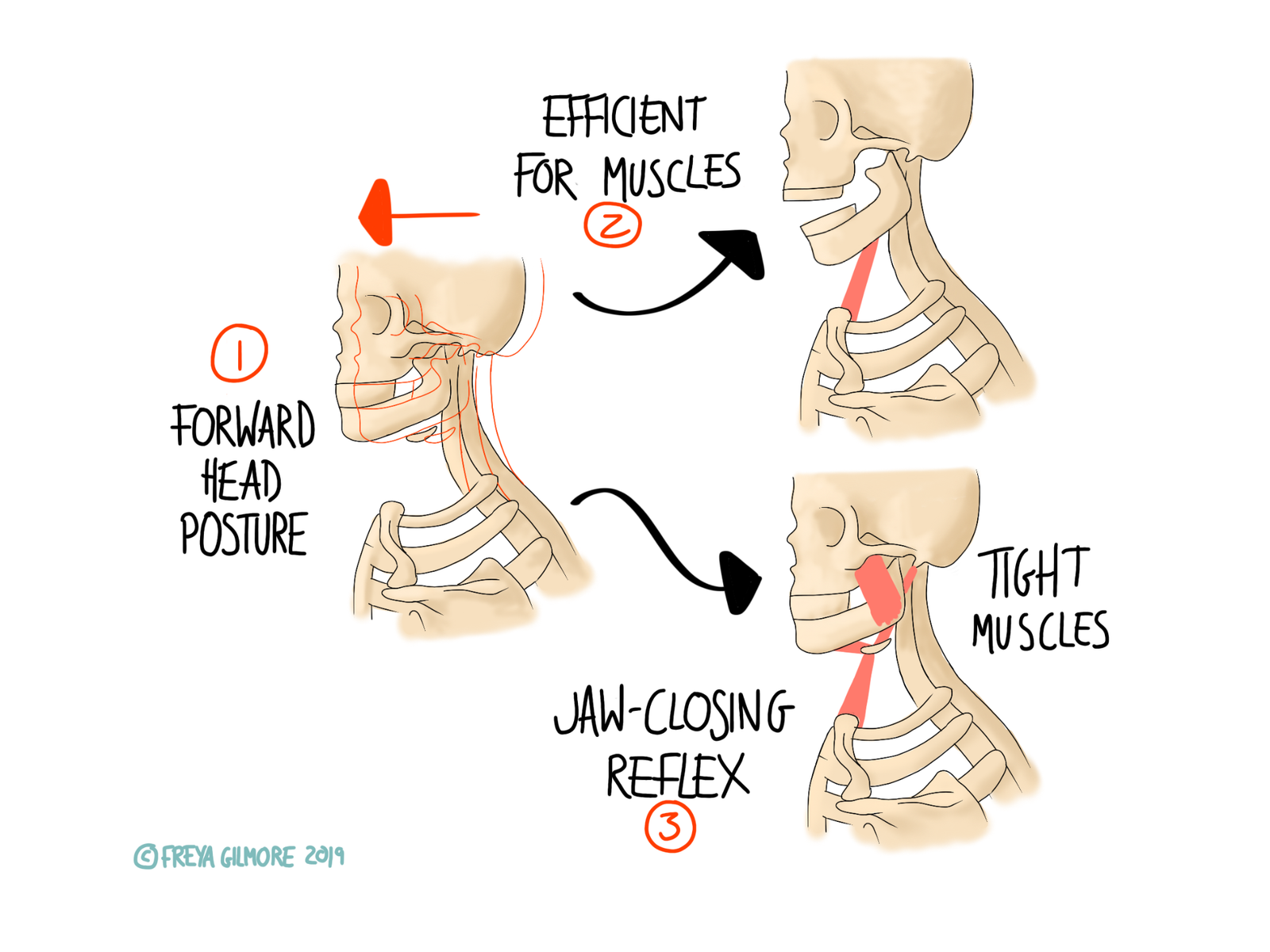
Osteopaths understand that everything in the body is connected. This even goes beyond muscles, joints,…
Rheumatic Pain
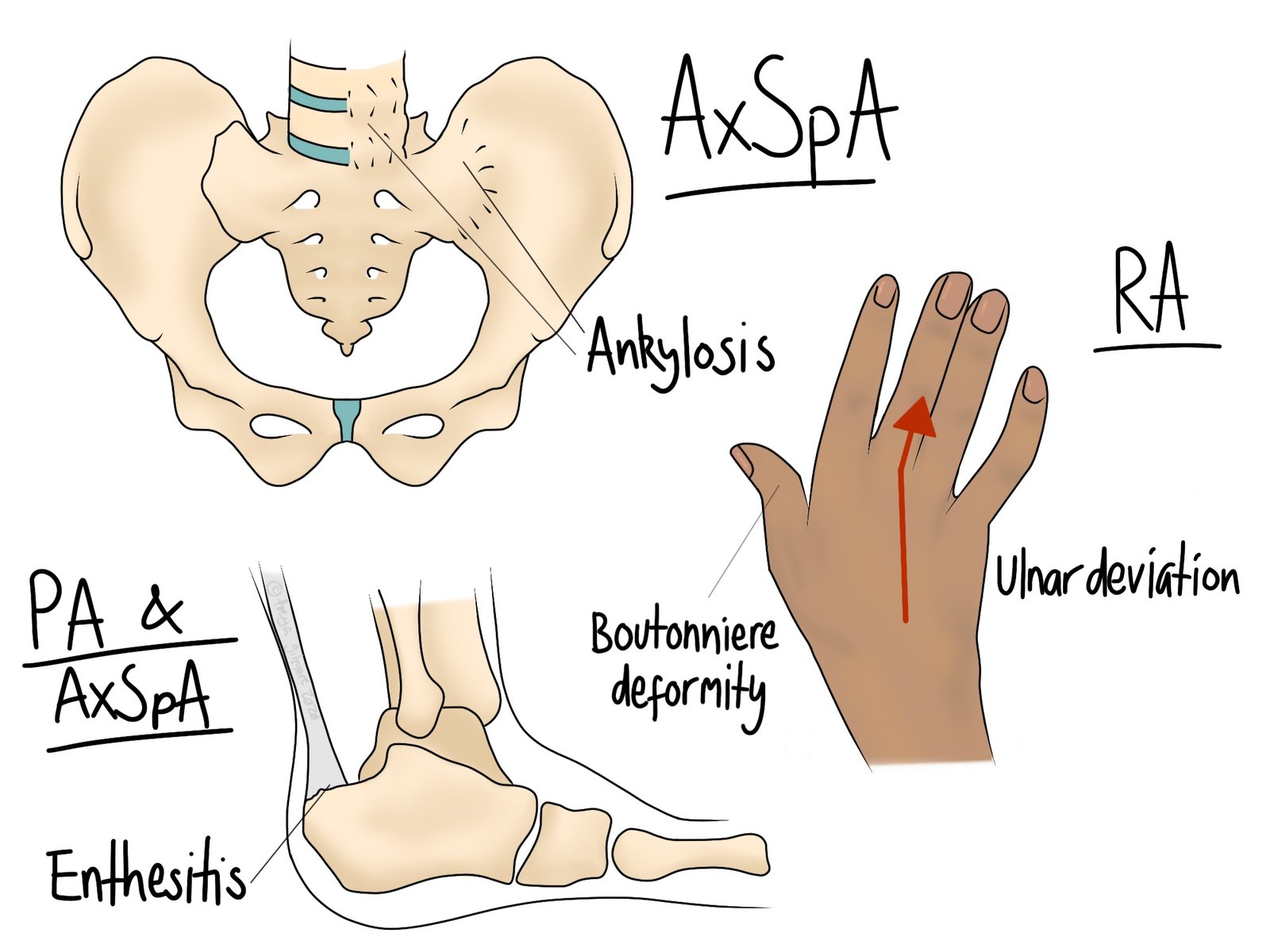
Rheumatic pain encompasses conditions such as rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. These are all autoimmune conditions that involve the body attacking its own joints. There is a lot of overlap between them, and the presence of one may make the diagnosis of another more likely. Osteoarthritis does not fall into this category.
Rheumatoid Arthritis (RA)
In RA, the hands and feet are typically the most affected. The small joints here become inflamed, and over time lead to specific deformities. As illustrated, the fingers may become bent into a “swan neck” deformity, and the wrist may cause the hand to deviate out to the side.
Symptoms usually begin subtly for no apparent reason, but sometimes they develop after an illness or infection. RA does not just affect the joints, it can also involve the eyes, heart, and lungs. Your osteopath may refer you back to the GP for blood tests and further investigations if RA is suspected. Early medication is recognised as providing the best outlook for long term progress.
Ankylosing Spondylitis (AS)
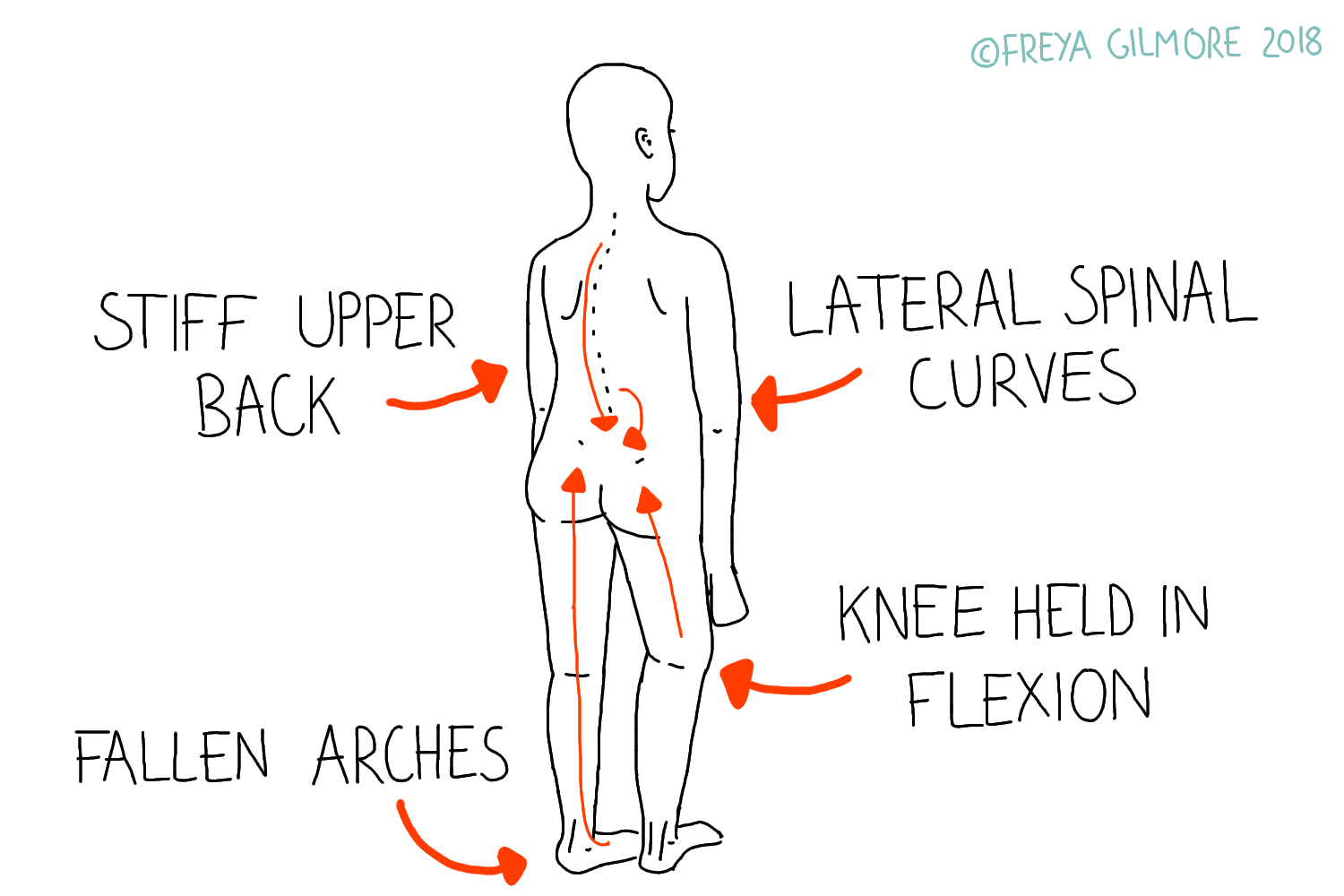
The lower back is affected in AS, where periods of inflammation cause damage to the joints. The body attempts to heal by laying down bone. Unfortunately this covers the joints themselves and gradually fuses them together. As the disease progresses, it causes stiffness and pain. If left unmanaged, the patient may develop a “?” shaped posture.
In the early stages, AS behaves quite similarly to typical back pain, but an early diagnosis is needed for the best outcomes. Symptoms are worse in the morning, and last more than half an hour after waking. They respond well to anti-inflammatory drugs such as ibuprofen or naproxen. Alongside the back pain, there may also be heel or finger pain or swelling. Family and personal medical history can also give clues. Conditions other forms of rheumatic arthritis or inflammatory bowel disease are associated with AS.
Your osteopath is in a good position to support you in reaching a specialist if you suspect your lower back pain might not be purely mechanical. AS can only be formally diagnosed by a rheumatologist.
Psoriatic Arthritis (PA)
Psoriatic Arthritis is a relatively common complication of psoriasis. It affects roughly 10% of people who have psoriasis. The joints affected may be in areas where psoriasis is more prevalent, or it may seem to be unrelated. It is possible in some cases for the arthritis to precede the development of psoriasis itself.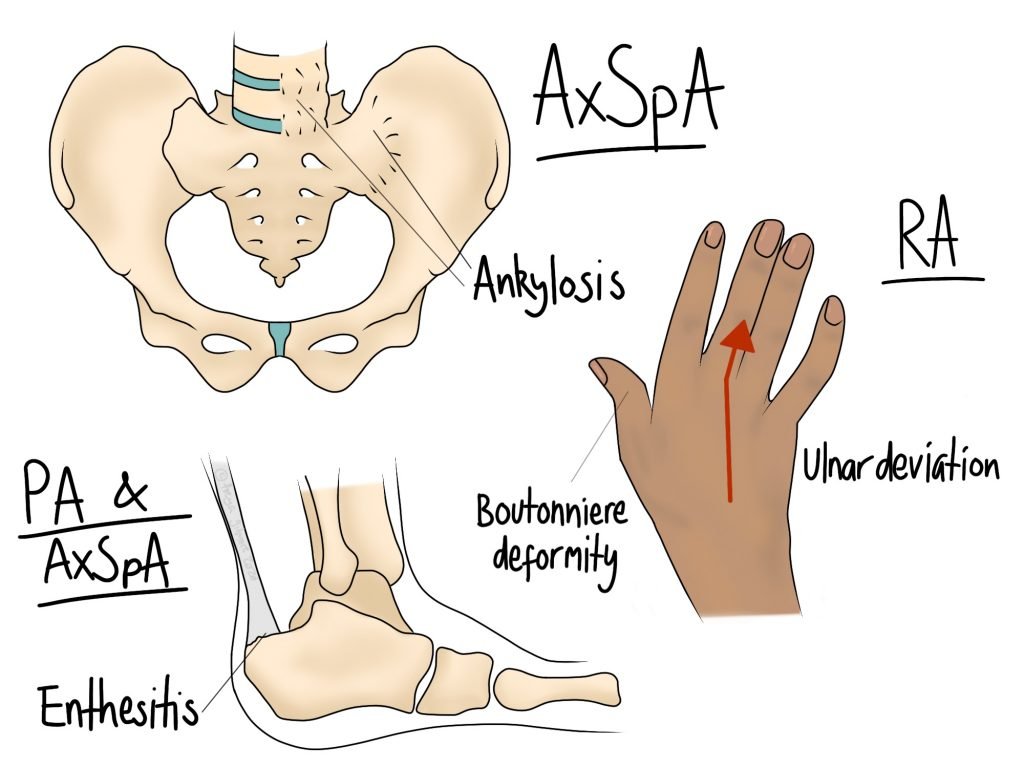
There is crossover with some of the symptoms shown in AS:
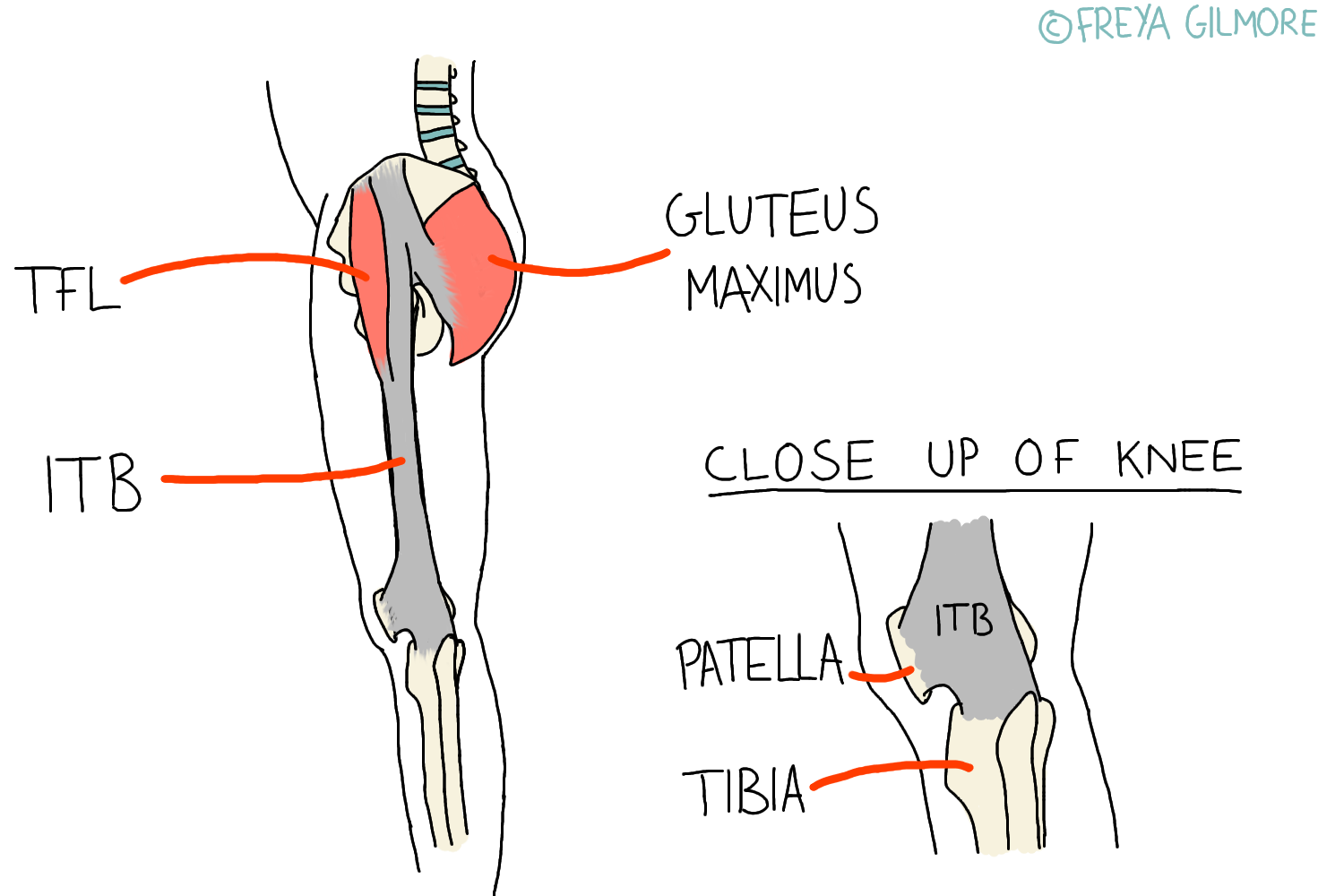
- Enthesitis. This is inflammation where tendons meet bone, such as the Achilles tendon at the heel.
- Dactylitis. A term for finger inflammation and “sausage digits”.
- Spondylitis and possible sacroiliitis. These are cases of inflammation at the spinal joints and pelvis.
However, not all of these symptoms may present in one person at the same time. You may want to keep a diary of symptoms if you find they come and go. Identifying a pattern is useful for both diagnosis and management.
Managing Rheumatic Symptoms
Rheumatic symptoms affecting the joints are often down to inflammation. We know that inflammation is worse with rest, which is why these conditions are associated with morning pain and stiffness lasting more than half an hour. However, inflammatory conditions are also worse with excessive activity. So there is a comfortable level of movement that allows for the lowest levels of symptoms. This is not to say that this movement will cure the condition, only provide symptomatic relief.
Many rheumatic symptoms behave similarly to more straight forward conditions. As a result, these conditions can be missed in their early stages. Your osteopath can support you in your referral to rheumatology if this is suspected.
Book now for symptomatic relief of rheumatic pain.