Osteopaths understand that everything in the body is connected. This even goes beyond muscles, joints,…

Hormones and Pain
Thankfully, we’re hearing a lot more about the wide reaching impacts the menopause can have. Changes in hormones can affect the way we feel pain, although this is not just limited to changes in the menopause. Thyroid hormones are well known to affect pain processing too.
Changes in Hormones During the Menopause
During the menopause, the body reduces output of a handful of hormones, including oestrogen and progesterone. Oestrogen is understood to be protective against pain; meaning that the presence of oestrogen in the body helps to reduce the pain you feel. Pain is multifactorial, and the menopausal drop of oestrogen will not have a significant effect on pain for everyone. But for some, it will be significant.
Fibromyalgia and Oestrogen
Fibromyalgia is an example of a chronic pain condition that affects women much more than men. A 2020 study found that women may also have more tender points than men. However, other features such as fatigue, brain fog, and depression presented similarly. Despite this, studies show a correlation between the onset, or worsening of fibromyalgia symptoms, and the menopause.
Bone Density
The reduction in oestrogen also adversely affects bone density. As a result, post-menopausal women are the demographic at highest risk of osteoporosis and osteopenia. Osteoporotic fractures can occur surprisingly easily, and it is not unusual for a diagnosis of osteoporosis to only occur following a fracture. Although this is a much more simple perspective, it is a significant part of how the menopause can be associated with musculoskeletal pain.
The Silver Lining
Despite all of this, a 2014 review found that while endometriosis and menstrual migraine are unsurprisingly improved by the menopause, positive or negative links to other chronic pain conditions are flimsy. It does acknowledge that ” the literature is highly suggestive of the role of ovarian hormones in modulating [chronic pain] conditions”
Thyroid Hormones and Pain
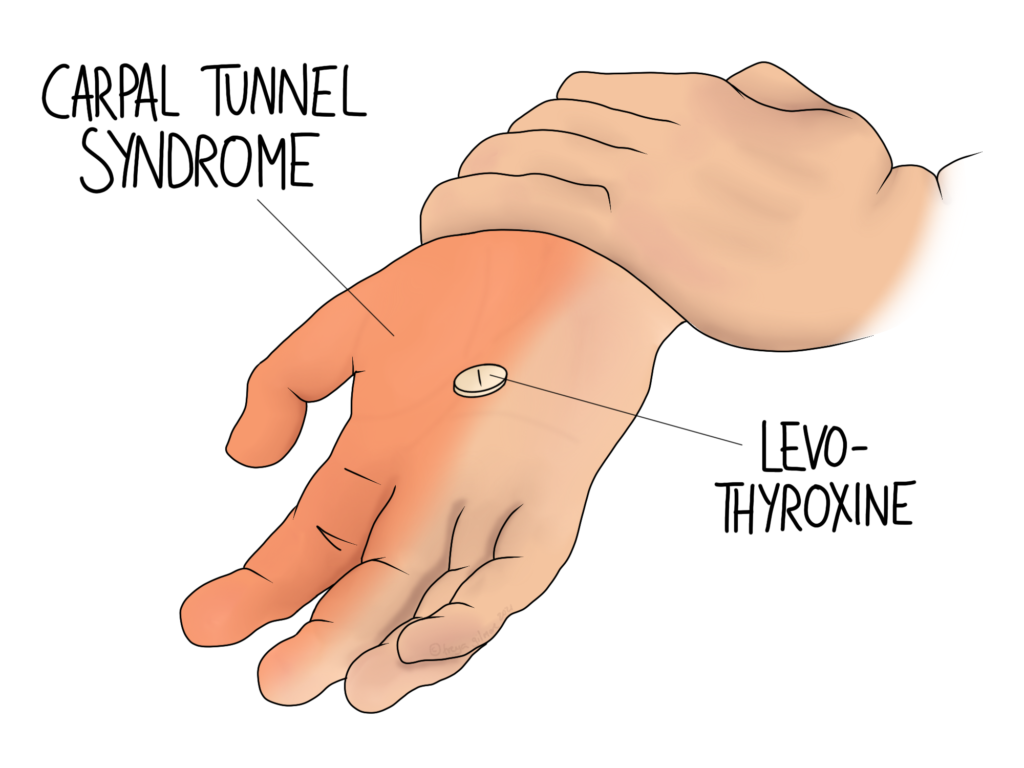
As the illustration above suggests, carpal tunnel syndrome can be associated with hypothyroidism. In fact, similarly to osteoporosis above, the earliest signs of hypothyroidism may appear to be musculoskeletal. Annoyingly, the exact reasons why hypothyroidism can seemingly cause carpal tunnel syndrome are unclear.
Around 5% of the general population are diagnosed with hypothyroidism, making it a relatively common ailment. Estimates suggest that another 5% may not be diagnosed, but fit the criteria for hypothyroidism. The pregnant and recently post-partum population may be of specific interest here: carpal tunnel syndrome is common in pregnancy, in association with fluid retention. Within 6 months of giving birth, postpartum thyroiditis can develop. This is rare, and first causes hyperthyroidism, before causing a drop. If you have noticed carpal tunnel symptoms coming and going, it may be worth getting a blood test to check your thyroid hormone levels.
Osteopathy and Hormonal Pain
Your osteopath will look at your case as a whole, taking a detailed history to pick up on details that may point to things like hormonal factors. Treating a thyroid-related case of carpal tunnel unsuccessfully, and referring back to your GP for surgery wouldn’t benefit anyone. But osteopaths have the luxury of time, and even if symptoms are still emerging, we are in a good position to spot the trends that might suggest the next step should be a blood test, not an operation.